Integrin alpha-6 in Prostate Cancer
1. Introduction
In Western populations, prostate cancer is one of the leading causes of cancer-related deaths in males, second only to lung cancer [1]. In 2015, the Australian Bureau of Statistics reported more than 18,000 incidences of prostate cancer, with over 3000 deaths [2]. Despite this, the frequency of relapse is still as high as 30% within 10 years of primary treatment [3][4][5] of which a large portion is owed to early micrometastatic progression in bone marrow [6]. Studies have shown that the five-year survival rate of patients with contained prostate cancer is more than triple that of their metastatic counterparts [7]. As such, early diagnosis of aggressive prostate cancer has enormous potential to improve survival and quality of life [8][9]. Currently, there are insufficient diagnostic tools to discriminate between indolent tumours and those with high propensity to metastasise. Therefore, there is a clinical imperative for novel molecular markers in the early identification of malignant potential, which could ultimately lead to the development of therapeutic interventions against cancer cell invasion and migration.
The existence of a stem cell subpopulation in the prostate has been well-documented and is proposed to reside within the basal cell compartment of the prostate gland [10][11]. Their ability to self-renew and undergo multiple-lineage differentiation has led to studies about their tumorigenic properties. Over the past decade, however, the existence of a minor subpopulation of tumour cells known as cancer stem cells (CSCs) has been proposed. These CSCs are titled accordingly due to their capacity for self-renewal and invasion, as well as their differential ability to recapitulate the phenotype of their primary tumour [12][13][14]. Their stem cell-like characteristics have been suggested to be responsible for solid tumorigenesis, metastasis and even some resistance to chemotherapy, as a response to their ability to divide asymmetrically [15][16][17][18][19]. Understandably, targeting abnormal CSCs will necessarily be preceded by specific knowledge of marker proteins expressed in this subpopulation.
To date, studies have identified several putative markers of prostate stem cells, including a number of adhesion molecules known as integrins [20][21][22]. Research surrounding integrin involvement in cancer biology, and particularly prostate cancer progression, has attracted significant interest in recent decades. This review focuses specifically on one integrin, integrin α6 (ITGA6/CD49f), in light of the growing body of evidence suggesting its implication in prostate cancer susceptibility, CSC biology and tumour cell migration and metastasis. The aim of this review is to convey an overview of the biological function of integrin α6, present current evidence about its diagnostic and prognostic value and ultimately discuss the potential role of this integrin as a future target for drug design.
2. Materials and Methods
2.1 Search strategy and inclusion criteria
An electronic search of the MEDLINE and EMBASE databases was performed using the following MeSH and other keywords: integrin alpha6, alpha 6, alpha-6, alpha6, ITGA6, prostate cancer and prostate neoplasms. The search was restricted to articles in the English language. There was no limitation for publication year. Abstract submissions and studies for which integrin alpha 6 was not the primary focus were excluded. Studies were selected for inclusion if they contained empirical research that investigated integrin α6 natin prostate cancers and then judged on their focus on integrin alpha-6 and contribution to the review.
Reference lists of all relevant articles were hand-searched for additional relevant studies. Titles and/or abstracts of relevant studies from this search strategy were screened by the author. Full-text articles were retrieved and screened when abstracts and titles were insufficient for determining inclusion or exclusion in the review.
3. Results
Eighteen relevant studies, published between 1994-2017 were included in this review. Six publications reported integrin α6 as a putative stem cell marker in prostate cancer, while two of the eighteen studies investigated its role in bony metastasis and invasion in a xenograft model. Five studies reported an association between increased expression of integrin α6 and metastatic progression and invasive phenotype of prostate cancer cell, although one study reported integrin α6 as a predictor of non-aggressive disease. Several studies were conducted by the same group of investigators.
Integrin α6 expression is persistent in invasive prostate cancer cell lines. The expression of this integrin is associated with aggressive phenotype, poor patient progression and increased metastasis. Its structural variant, integrin α6p is also reported to contribute to invasion and migration of prostate tumour cells on laminin.
4. Discussion
4.1 Structure of prostate – normal and neoplastic
The normal prostatic epithelium comprises of pseudostratified layers of luminal, basal and neuroendocrine cells [23] which form part of a duct-acinar system [24][25]. These secretory epithelial cells are supported by the basal lamina, found at the epithelium-stroma interface [26][27][28]. The significance of the basal lamina is two-fold; a) structurally, it represents a physical barrier which must be breached in the context of metastasis [29][30][31] and b) functionally, its molecular composition of proteoglycans, collagens and non-collagenous glycoproteins such as laminin [32] lend it to involvement in cellular processes such as attachment, migration and differentiation [33][34]. This is consistent with evidence of altered composition, such as loss of collagen type VII [32][35] and laminin B2t [36] in neoplastic basal lamina.
Currently, the exact cellular origin of CSCs is still widely debated. The greater expression of luminal cell markers on prostate cancer cells than basal cell markers has led to the hypothesis that prostate cancer arises from terminally differentiated luminal cells [37][38]. However, there is also a belief that intermediate progenitors [39][40] or subpopulations of multipotent stem cells from the basal epithelial layer may give rise to prostate cancer instead [41][42]. Consequently, there still exists a paucity of accepted techniques used to characterize and isolate CSCs in prostate cancer tissue.
4.2 Structure and biological function of integrin-α6
Integrins are a large group of heterodimeric transmembrane glycoproteins that mediate interactions between cells and extracellular matrix (ECM) through molecular adhesion. They are comprised of one α subunit and one β subunit, which together determine ligand specificity and facilitate bidirectional signaling upon activation by ligands [43]. Each subunit contains an extracellular domain for ligand attachment, a transmembrane domain and a short tail within the cytoplasm [44]. This cytoplasmic tail interaction allows integrins to serve as sensors of dimensionality within the matrix [45] and transduce mechanical forces from the ECM into biochemical survival signals, resulting in the inhibition of a p53-regulated apoptotic pathway [46][47]. Upon ligand binding, integrins complex with the cell membrane to form focal adhesions, consisting of signaling and adaptor proteins [48][49]. These in turn engage relevant kinases to initiate downstream intracellular signaling cascades [44] such as the focal adhesion kinase (FAK) and the phosphatidylinositol 3-kinase (PI3K)/AKT pathways [50][51] and thus regulate proliferation, migration, invasion and cell migration [45]. Additionally, crosstalk between the activation of AKT and p53 degradation via phosphorylation of Mdm2 has been discovered [52][53]. Integrins play a critical role in numerous biological events involving ECM remodeling, including wound healing and embryonic development [54].
4.3 Integrin α6 structure
One integrin that has raised particular interest in the framework of prostate cancer progression is integrin α6. This mechanosensing integrin is encoded by the ITGα6 gene, and dimerizes with β1 or β4 chains to form either α6β1 or α6β4 complexes, respectively [55]. Both of these serve as receptors for the laminin family of ECM proteins, despite differing expressions and roles. α6β1 is widely expressed in epithelia and associated with strong anchorage and stabilization of skin tissue through hemidesmosome formation [56][57]. α6β4 is involved in cellular migration such as embryogenic organ and tissue development [58][59] and prominently identified on platelets, macrophages, lymphocytes and many epithelial cells [60].
4.4 Integrin-α6 function, regulation and expression
The major function of laminin-binding integrin-α6 is maintaining stable anchorage and structural integrity of skin and glandular epithelium whilst withstanding mechanical and shear stresses [61]. Mutations of the ITGα6 gene has been associated with basement separation and epithelial blistering of varying severity [62][63][64]. In the context of CSCs, integrin-α6 has also been demonstrated to play a key regulatory role in self-renewal, proliferation and tumour-formation capacity in glioblastoma stem cells cervical uterine cancer cells [65][66].
Despite its important role in CSCs, there is a shortage in understanding of the molecular mechanisms involved in the regulation of integrin-α6. The limited current knowledge surrounding the stem cell self-renewal control by integrin-α6 derives mainly from studies in embryonic stem cells (ESCs) and breast CSCs. OCT4 and SOX2 are two pluripotent-related genes which maintain the self-renewal capacity of undifferentiated ESCs (67). Yu et al. (2012) revealed that increased expression of OCT4 and SOX2 led to upregulation of integrin-α6 expression, and demonstrated the regulation of integrin-α6 through the direct binding of OCT4 and SOX2 on specific regions of the integrin-α6 promoter [68].
In normal prostatic tissue, the basal lamina boasts a great diversity of molecular components, including collagen IV, VII, entactin, fibronectin, vitronectin, tenascin, laminin 5, 6, 7 (containing the α3 chain) and laminin 10-11 (containing α5 chain) [32][69]. Integrin-α6 is just one of a wide range of integrin receptor units which are polarised on the basal cell layer, adjacent to the basal lamina.
In human prostatic carcinoma, however, all but a select few components of the basal lamina are lost. As a result, there is a significant loss of the corresponding integrin units [70] which is consistent with the lack of integrin subunits observed on the tumour cell surface of invasive prostate carcinomas [36]. The α6 integrin is a notable exception to this, demonstrating a persistent expression in 69% of invasive prostate carcinomas [70].
4.5 Integrin-α6 expression and patient prognosis
In human prostate cancer, integrin α6 expression is preserved in a diffuse manner on the plasma membrane, rather than being polarised on the basal layers [36]. The progression of prostate tumour development generally begins with the emergence of precursor prostatic intraepithelial neoplasia lesions, followed by carcinoma in situ and eventually, extracapsular invasion into neighbouring structures and distant metastases sites [36]. Overwhelmingly, current evidence supports the theory that elevated expression of integrin α6β1 is correlated with an aggressive phenotype during tumour progression, poor patient prognosis and increased metastasis [6][71][72][73][74].
Rabinovitz, Nagle & Cress (1995) investigated the invasive phenotypic features of human prostate carcinoma cells by comparing the α6-high with α6-low cell subpopulations. In vitro assays were used to demonstrate a significantly higher rate of random migration on coated laminin in the α6-high sublines as compared with the α6-low sublines. α6-antibodies were then used to confirm the involvement of α6, and particularly α6β1, as it was the primary distinguisher between α6-high with α6-low cells.
Severely compromised immunodeficient mice were then used to assess the invasion and migration capacity of the α6 sublines in vivo. α6-high subpopulations were found to exhibit a significantly higher rate of invasion through the laminin-rich mice diaphragm, as characterized by several basement membrane breaching points. These findings are consistent with evidence suggesting an association between increasing prostatic intraepithelial neoplasia grades and progressive basal cell disruption [75].
This could be partially explained by the role of the integrin-ECM interaction in providing traction for tumour cell invasion during dissociation of the cell from ECM proteins at the leading edge of the cell migratory path [76][77] or the extracapsular escape facilitated by laminin-coated nerves [72]. However, this is conflicted by some evidence noting an association between high expression levels of integrin α6 and lowered recurrence rate, disease-associated death following radical prostatectomy, as well as other non-aggressive tumour features such as low Gleason score (<7), serum PSA levels of 10ng/mL and pT2 stage [78]. Integrin α6 has also been shown to be a predictor of biochemical and local recurrence of prostate cancer [79].
More recently, a novel structural variant of integrin α6, called integrin α6p has been identified [7]. This is formed by post-translational proteolytic cleavage of the ligand-binding extracellular domain by urokinase-type plasminogen activator (uPA) on the tumour cell surface [70][80]. The cleavage of integrin α6 contributes to invasion and migration of the tumour cell on laminin, whilst in vitro and in vivo studies of integrin α6p have shown that inhibition of the cleavage function significantly hinders tumour migration within the bone [81][82] and encourages the formation of curative-type bone lesions [73][83][84]. These results highlight the prevention of integrin α6p production as a potential novel treatment strategy for delaying disease progression within the bone.
4.6 Integrin-targeted modalities for prostate cancer treatment in lab and future directions
Given the growing recognition of integrins’ roles in facilitating prostate cancer invasion and metastasis, there has been increasing research into future treatment modalities targeted at these adhesion molecules. Various groups have developed pre-clinical models to investigate the functional significance of targeting integrin α6. For example, King 2008 demonstrated the reduced tumour cell migration and onset and degree of bone pain and fractures in xenograft mouse models injected with uncleaved integrin α6 (α6pB1) as compared with cleaved (α6B1) [85]. A similar model has since been used by Landowski 2014, in testing an integrin α6 functional blocking monoclonal antibody, called J8H [6]. The results of this study showed promising outcomes of J8H in blocking tumour progression and subsequently improving survival outcomes without impacting cell adhesion to laminin. Despite this, currently there are only four drugs that have passed Phase II trial for treatment of metastatic prostate cancer (Cilengitide, Etaracizumab, Intetumumab and Abituzumab) [86]. One reason for this limited number of integrin antibodies in clinical trial is the difficulty posed by their bidirectional nature of cell signalling, as targeting these integrins may lead to the altered expression and function of other receptors [86]. Furthermore, most integrins are not constitutively active, and therefore, change their expression in response to changes in external stimuli, including therapy. This complicates integrin antagonism, and could limit clinical effectiveness of targeted therapy.
5. Conclusion
The need for early detection and prevention of tumour cell metastasis drives the search for greater diagnostic and prognostic biomarkers in prostate cancer. Integrin-targeted treatment presents as a promising area in which drug development may have a significant impact on patient survival. There is still much to learn about the role of integrins in prostate tumour cell migration and invasion, and the clinical significance of integrin inhibition in prostate cancer is still unclear. Whilst the pool of preclinical evidence supporting a role for integrin α6 in prostate cancer invasion, future clinical studies of bony metastasis prevention via integrin inhibition are required. Combined therapy of integrin treatment with radiotherapy is also a consideration for future research, as it has the potential to increase prostate tumour sensitivity to radiation and drug therapies [87]. A greater understanding of integrin signalling and expressional changes modulates our prospects of developing targeted biological interventions to slow prostate cancer progression.
Supplementary Materials: Not applicable
Acknowledgments: Not applicable
Author Contributions: Not applicable
Conflicts of Interest: The author declares no conflict of interest
6. References
[1] Society AC. Cancer Facts & Figures 2013. Atlanta: American Cancer Society 2013; 2013.
[2] Statistics ABo. 3303.0 – Causes of Death, Australia, 2015 2016 [updated 26 September 2017.
[3] Boorjian SA, Karnes RJ, Viterbo R, Rangel LJ, Bergstralh EJ, Horwitz EM, et al. Long-term survival after radical prostatectomy versus external-beam radiotherapy for patients with high-risk prostate cancer. Cancer. 2011;117(13):2883-91.
[4] Thobe M, Clark R, Bainer R, Prasad S, Rinker-Schaeffer C. From Prostate to Bone: Key Players in Prostate Cancer Metastasis. Cancers. 2011;3(1):478-93.
[5] Liu W, Laitinen S, Khan S, Vihinen M, Kowalski J, Yu G, et al. Copy number analysis indicates monoclonal origin of lethal metastatic prostate cancer.[Erratum appears in Nat Med. 2009 Jul;15(7):819]. Nat Med. 2009;15(5):559-65.
[6] Landowski TH, Gard J, Pond E, Pond GD, Nagle RB, Geffre CP, et al. Targeting integrin alpha6 stimulates curative-type bone metastasis lesions in a xenograft model. Mol Cancer Ther. 2014;13(6):1558-66.
[7] Kacsinta AD, Rubenstein CS, Sroka IC, Pawar S, Gard JM, Nagle RB, et al. Intracellular modifiers of integrin alpha 6p production in aggressive prostate and breast cancer cell lines. Biochem Biophys Res Commun. 2014;454(2):335-40.
[8] Morris MJ, Scher HI. Clinical approaches to osseous metastases in prostate cancer. Oncologist. 2003;8(2):161-73.
[9] Sturge J, Caley MP, Waxman J. Bone metastasis in prostate cancer: emerging therapeutic strategies. Nat Rev Clin Oncol. 2011;8(6):357-68.
[10] De Marzo AM, Nelson WG, Meeker AK, Coffey DS. Stem cell features of benign and malignant prostate epithelial cells. J Urol. 1998;160(6 Pt 2):2381-92.
[11] Huang CK, Luo J, Lee SO, Chang C. Concise review: androgen receptor differential roles in stem/progenitor cells including prostate, embryonic, stromal, and hematopoietic lineages. Stem Cells. 2014;32(9):2299-308.
[12] Eaton CL, Colombel M, Van Der Pluijm G, Cecchini M, Wetterwald A, Lippitt J, et al. Evaluation of the frequency of putative prostate cancer stem cells in primary and metastatic prostate cancer. Prostate. 2010;70(8):875-82.
[13] Liao CP, Adisetiyo H, Liang M, Roy-Burman P. Cancer-associated fibroblasts enhance the gland-forming capability of prostate cancer stem cells. Cancer Res. 2010;70(18):7294-303.
[14] Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ. Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res. 2005;65(23):10946-51.
[15] Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8(10):755-68.
[16] Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells.[Erratum appears in Proc Natl Acad Sci U S A. 2003 May 27;100(11):6890]. Proc Natl Acad Sci U S A. 2003;100(7):3983-8.
[17] Tan BT, Park CY, Ailles LE, Weissman IL. The cancer stem cell hypothesis: a work in progress. Laboratory Investigation. 2006;86(12):1203-7.
[18] Liu W, Moulay M, Willenbrock S, Roolf C, Junghanss C, Ngenazahayo A, et al. Comparative characterization of stem cell marker expression, metabolic activity and resistance to doxorubicin in adherent and spheroid cells derived from the canine prostate adenocarcinoma cell line CT1258. Anticancer Res. 2015;35(4):1917-27.
[19] Fedr R, Pernicova Z, Slabakova E, Strakova N, Bouchal J, Grepl M, et al. Automatic cell cloning assay for determining the clonogenic capacity of cancer and cancer stem-like cells. Cytometry A. 2013;83(5):472-82.
[20] Goldstein AS, Lawson DA, Cheng D, Sun W, Garraway IP, Witte ON. Trop2 identifies a subpopulation of murine and human prostate basal cells with stem cell characteristics. Proc Natl Acad Sci U S A. 2008;105(52):20882-7.
[21] Collins AT, Habib FK, Maitland NJ, Neal DE. Identification and isolation of human prostate epithelial stem cells based on alpha(2)beta(1)-integrin expression. J Cell Sci. 2001;114(Pt 21):3865-72.
[22] Richardson GD, Robson CN, Lang SH, Neal DE, Maitland NJ, Collins AT. CD133, a novel marker for human prostatic epithelial stem cells. J Cell Sci. 2004;117(Pt 16):3539-45.
[23] Strand DW, Goldstein AS. The many ways to make a luminal cell and a prostate cancer cell. Endocr Relat Cancer. 2015;22(6):T187-97.
[24] Petkova N, Hennenlotter J, Sobiesiak M, Todenhofer T, Scharpf M, Stenzl A, et al. Surface CD24 distinguishes between low differentiated and transit-amplifying cells in the basal layer of human prostate. Prostate. 2013;73(14):1576-90.
[25] Ware JL. Prostate cancer progression. Implications of histopathology. Am J Pathol. 1994;145(5):983-93.
[26] Nagle RB, Brawer MK, Kittelson J, Clark V. Phenotypic relationships of prostatic intraepithelial neoplasia to invasive prostatic carcinoma. Am J Pathol. 1991;138(1):119-28.
[27] Bonkhoff H, Wernert N, Dhom G, Remberger K. Basement membranes in fetal, adult normal, hyperplastic and neoplastic human prostate. Virchows Arch A Pathol Anat Histopathol. 1991;418(5):375-81.
[28] Bonkhoff H, Wernert N, Dhom G, Remberger K. Distribution of basement membranes in primary and metastatic carcinomas of the prostate. Hum Pathol. 1992;23(8):934-9.
[29] Liotta LA, Rao CN, Wewer UM. Biochemical interactions of tumor cells with the basement membrane. Annu Rev Biochem. 1986;55:1037-57.
[30] Nakajima M, Welch DR, Irimura T, Nicolson GL. Basement membrane degradative enzymes as possible markers of tumor metastasis. Prog Clin Biol Res. 1986;212:113-22.
[31] Tryggvason K, Hoyhtya M, Salo T. Proteolytic degradation of extracellular matrix in tumor invasion. Biochim Biophys Acta. 1987;907(3):191-217.
[32] Knox JD, Cress AE, Clark V, Manriquez L, Affinito KS, Dalkin BL, et al. Differential expression of extracellular matrix molecules and the alpha 6-integrins in the normal and neoplastic prostate. Am J Pathol. 1994;145(1):167-74.
[33] Ekblom P. Developmentally regulated conversion of mesenchyme to epithelium. Faseb J. 1989;3(10):2141-50.
[34] Hay E. Extracellular matrix, cell skeletons, and embryonic development. American Journal of Medical Genetics. 1989;34(1):14-29.
[35] Fuchs ME, Brawer MK, Rennels MA, Nagle RB. The relationship of basement membrane to histologic grade of human prostatic carcinoma. Modern Pathology. 1989;2(2):105-11.
[36] Cress AE, Rabinovitz I, Zhu W, Nagle RB. The alpha 6 beta 1 and alpha 6 beta 4 integrins in human prostate cancer progression. Cancer Metastasis Rev. 1995;14(3):219-28.
[37] Wang X, Kruithof-de Julio M, Economides KD, Walker D, Yu H, Halili MV, et al. A luminal epithelial stem cell that is a cell of origin for prostate cancer. Nature. 2009;461(7263):495-500.
[38] Collins AT, Maitland NJ. Prostate cancer stem cells. Eur J Cancer. 2006;42(9):1213-8.
[39] De Marzo AM, Meeker AK, Zha S, Luo J, Nakayama M, Platz EA, et al. Human prostate cancer precursors and pathobiology. Urology. 2003;62(5 Suppl 1):55-62.
[40] van Leenders GJ, Schalken JA. Epithelial cell differentiation in the human prostate epithelium: implications for the pathogenesis and therapy of prostate cancer. Crit Rev Oncol Hematol. 2003;46 Suppl:S3-10.
[41] Goldstein AS, Huang J, Guo C, Garraway IP, Witte ON. Identification of a cell of origin for human prostate cancer. Science. 2010;329(5991):568-71.
[42] Taylor RA, Toivanen R, Frydenberg M, Pedersen J, Harewood L, Australian Prostate Cancer B, et al. Human epithelial basal cells are cells of origin of prostate cancer, independent of CD133 status.[Erratum appears in Stem Cells. 2012 Aug;30(8):1786 Note: ]. Stem Cells. 2012;30(6):1087-96.
[43] Lowin T, Straub RH. Integrins and their ligands in rheumatoid arthritis. Arthritis Research & Therapy. 2011;13(5):244.
[44] Chamberlain MC, Cloughsey T, Reardon DA, Wen PY. A novel treatment for glioblastoma: integrin inhibition. Expert Review of Neurotherapeutics. 2012;12(4):421-35.
[45] Larsen M, Artym VV, Green JA, Yamada KM. The matrix reorganized: extracellular matrix remodeling and integrin signaling. Current Opinion in Cell Biology. 2006;18(5):463-71.
[46] Ilic D, Almeida EA, Schlaepfer DD, Dazin P, Aizawa S, Damsky CH. Extracellular matrix survival signals transduced by focal adhesion kinase suppress p53-mediated apoptosis. J Cell Biol. 1998;143(2):547-60.
[47] Shyy JY, Chien S. Role of integrins in cellular responses to mechanical stress and adhesion. Current Opinion in Cell Biology. 1997;9(5):707-13.
[48] Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110(6):673-87.
[49] Legate KR, Wickstr\”om SA, F\”assler R. Genetic and cell biological analysis of integrin outside-in signaling. Genes & Development. 2009;23(4):397-418.
[50] Koul D, Shen R, Bergh S, Lu Y, de Groot JF, Liu TJ, et al. Targeting integrin-linked kinase inhibits Akt signaling pathways and decreases tumor progression of human glioblastoma. Mol Cancer Ther. 2005;4(11):1681-8.
[51] Gambaletta D, Marchetti A, Benedetti L, Mercurio AM, Sacchi A, Falcioni R. Cooperative signaling between alpha(6)beta(4) integrin and ErbB-2 receptor is required to promote phosphatidylinositol 3-kinase-dependent invasion. J Biol Chem. 2000;275(14):10604-10.
[52] Oren M. Decision making by p53: life, death and cancer. Cell Death Differ. 2003;10(4):431-42.
[53] Ogawara Y, Kishishita S, Obata T, Isazawa Y, Suzuki T, Tanaka K, et al. Akt enhances Mdm2-mediated ubiquitination and degradation of p53. J Biol Chem. 2002;277(24):21843-50.
[54] Hynes RO. Integrins: versatility, modulation, and signaling in cell adhesion. Cell. 1992;69(1):11-25.
[55] Chen H, Qu J, Huang X, Kurundkar A, Zhu L, Yang N, et al. Mechanosensing by the a6-integrin confers an invasive fibroblast phenotype and mediates lung fibrosis. Nature Communications. 2016;7:12564.
[56] Nievers MG, Schaapveld RQ, Sonnenberg A. Biology and function of hemidesmosomes. Matrix Biology. 1999;18(1):5-17.
[57] Dowling J, Yu QC, Fuchs E. Beta4 integrin is required for hemidesmosome formation, cell adhesion and cell survival. The Journal of Cell Biology. 1996;134(2):559-72.
[58] Bronner-Fraser M, Artinger M, Muschler J, Horwitz AF. Developmentally regulated expression of alpha 6 integrin in avian embryos. Development. 1992;115(1):197-211.
[59] Damsky C, Sutherland A, Fisher S. Extracellular matrix 5: adhesive interactions in early mammalian embryogenesis, implantation, and placentation. FASEB Journal. 1993;7(14):1320-9.
[60] Feich ME, Willis RA, Penney DP, Keng PC, Phipps RP. Expression of alpha 6 beta 1 integrin, the laminin receptor, on subsets of normal murine lung fibroblasts and its upregulation by the inflammatory cytokines IFN-gamma and TNF-alpha. Regional Immunology. 1992;4(6):363-70.
[61] Harryman WL, Hinton JP, Rubenstein CP, Singh P, Nagle RB, Parker SJ, et al. The Cohesive Metastasis Phenotype in Human Prostate Cancer. Biochimica et Biophysica Acta – Reviews on Cancer. 2016;1866(2):221-31.
[62] Rashid KA, Stern JN, Ahmed AR. Identification of an epitope within human integrin alpha 6 subunit for the binding of autoantibody and its role in basement membrane separation in oral pemphigoid. J Immunol. 2006;176(3):1968-77.
[63] Mignogna M, Lanza A, Rossiello L, Ruocco V, Ahmed AR. Comparison of reactivity and epitope recognition between sera from American and Italian patients with oral pemphigoid. Clin Exp Immunol. 2006;145(1):28-35.
[64] Domogatskaya A, Rodin S, Tryggvason K. Functional diversity of laminins. Annu Rev Cell Dev Biol. 2012;28:523-53.
[65] Lathia JD, Gallagher J, Heddleston JM, Wang J, Eyler CE, Macswords J, et al. Integrin alpha 6 regulates glioblastoma stem cells. Cell Stem Cell. 2010;6(5):421-32.
[66] Ortiz-Sanchez E, Santiago-Lopez L, Cruz-Dominguez VB, Toledo-Guzman ME, Hernandez-Cueto D, Muniz-Hernandez S, et al. Characterization of cervical cancer stem cell-like cells: phenotyping, stemness, and human papilloma virus co-receptor expression. Oncotarget. 2016;7(22):31943-54.
[67] Iovino N, Cavalli G. Rolling ES cells down the Waddington landscape with Oct4 and Sox2. Cell. 2011;145(6):815-7.
[68] Yu KR, Yang SR, Jung JW, Kim H, Ko K, Han DW, et al. CD49f enhances multipotency and maintains stemness through the direct regulation of OCT4 and SOX2. Stem Cells. 2012;30(5):876-87.
[69] Brar PK, Dalkin BL, Weyer C, Sallam K, Virtanen I, Nagle RB. Laminin alpha-1, alpha-3, and alpha-5 chain expression in human prepubertal [correction of prepubetal] benign prostate glands and adult benign and malignant prostate glands. Prostate. 2003;55(1):65-70.
[70] Demetriou MC, Cress AE. Integrin clipping: a novel adhesion switch? J Cell Biochem. 2004;91(1):26-35.
[71] Schmelz M, Cress AE, Scott KM, Burger F, Cui H, Sallam K, et al. Different phenotypes in human prostate cancer: alpha6 or alpha3 integrin in cell-extracellular adhesion sites. Neoplasia. 2002;4(3):243-54.
[72] Ports MO, Nagle RB, Pond GD, Cress AE. Extracellular engagement of alpha6 integrin inhibited urokinase-type plasminogen activator-mediated cleavage and delayed human prostate bone metastasis. Cancer Res. 2009;69(12):5007-14.
[73] Sroka IC, Chopra H, Das L, Gard JM, Nagle RB, Cress AE. Schwann Cells Increase Prostate and Pancreatic Tumor Cell Invasion Using Laminin Binding A6 Integrin. J Cell Biochem. 2016;117(2):491-9.
[74] Sroka IC, Sandoval CP, Chopra H, Gard JM, Pawar SC, Cress AE. Macrophage-dependent cleavage of the laminin receptor alpha6beta1 in prostate cancer. Mol Cancer Res. 2011;9(10):1319-28.
[75] Bostwick DG, Qian J. High-grade prostatic intraepithelial neoplasia. Mod Pathol. 2004;17(3):360-79.
[76] Desgrosellier JS, Cheresh DA. Integrins in cancer: Biological implications and therapeutic opportunities. Nature Reviews Cancer. 2010;10(1):9-22.
[77] Millard M, Odde S, Neamati N. Integrin Targeted Therapeutics. Theranostics. 2011;1:154-88.
[78] Hoogland AM, Verhoef EI, Roobol MJ, Schroder FH, Wildhagen MF, Van Der Kwast TH, et al. Validation of stem cell markers in clinical prostate cancer: alpha6-Integrin is predictive for non-aggressive disease. Prostate. 2014;74(5):488-96.
[79] Hoogland AM, Verhoef EI, Roobol MJ, Schroder FH, Wildhagen MF, van der Kwast TH, et al. Validation of stem cell markers in clinical prostate cancer: alpha6-integrin is predictive for non-aggressive disease. Prostate. 2014;74(5):488-96.
[80] Demetriou MC, Pennington ME, Nagle RB, Cress AE. Extracellular alpha 6 integrin cleavage by urokinase-type plasminogen activator in human prostate cancer. Exp Cell Res. 2004;294(2):550-8.
[81] Pawar SC, Demetriou MC, Nagle RB, Bowden GT, Cress AE. Integrin alpha6 cleavage: a novel modification to modulate cell migration. Exp Cell Res. 2007;313(6):1080-9.
[82] Ports MO, Nagle RB, Pond GD, Cress AE. Extracellular engagement of alpha6 integrin inhibited urokinase-type plasminogen activator-mediated cleavage and delayed human prostate bone metastasis. Cancer Res. 2009;69(12):5007-14.
[83] Sroka IC, Anderson TA, McDaniel KM, Nagle RB, Gretzer MB, Cress AE. The laminin binding integrin alpha6beta1 in prostate cancer perineural invasion. Journal of Cellular Physiology. 2010;224(2):283-8.
[84] Deborde S, Omelchenko T, Lyubchik A, Zhou Y, He S, McNamara WF, et al. Schwann cells induce cancer cell dispersion and invasion. J Clin Invest. 2016;126(4):1538-54.
[85] King TE, Pawar SC, Majuta L, Sroka IC, Wynn D, Demetriou MC, et al. The role of alpha 6 integrin in prostate cancer migration and bone pain in a novel xenograft model. PLoS ONE. 2008;3(10):e3535.
[86] Philippe CL. Therapeutic value of an integrin antagonist in prostate cancer. Current Drug Targets. 2016;17(3):321-7.
[87] Weis SM, Cheresh DA. alphaV integrins in angiogenesis and cancer. Cold Spring Harb Perspect Med. 2011;1(1):a006478.
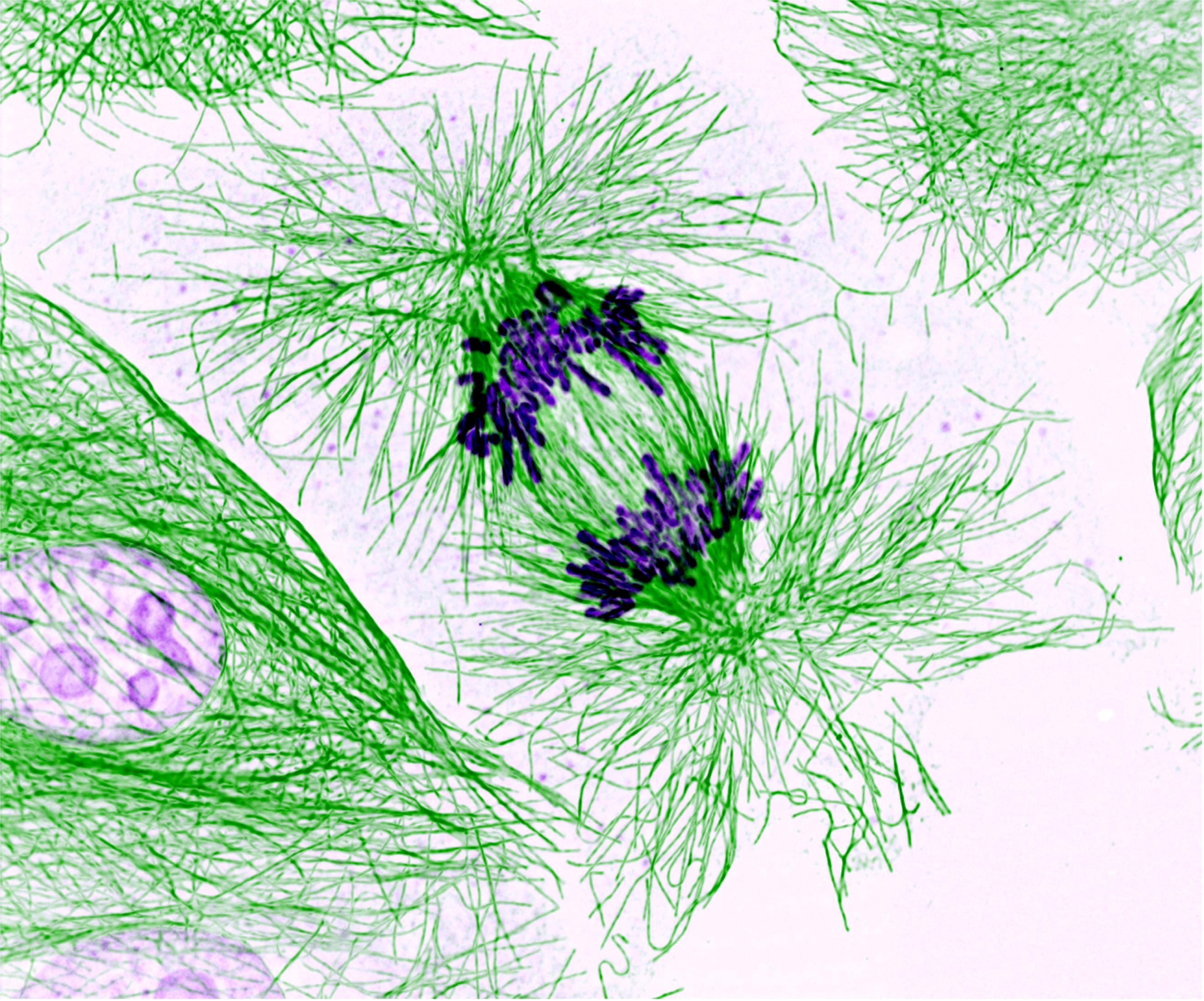
Article photo credit: Zeiss Microscopy
- Log in to post comments










