Continuity of Care in Elective Hernia Repair Surgery

1. Introduction
In the UK, the process of streamlining access to elective surgery can mean that a patient will discuss treatment with one medical professional in an outpatient setting, while the operation is carried out by a different individual surgeon. Relatively little is known about the differing perceptions of patients and surgeons relating to this issue, and while much research has been done on the significance of continuity of care in other settings, the impact in elective day case surgery is much less well understood. For example, orthopaedics patients awaiting joint arthroplasty reported that given the choice, they would be unlikely to change their surgeon for another, in order to receive a shorter waiting time [1]. We decided to investigate whether this view was similar in inguinal hernia repair surgery and whether patients would accept a longer waiting time for the same surgeon.
2. Methods
In order to investigate whether this view was the same for patients awaiting inguinal hernia repair surgery, a prospective study was undertaken. Two nine-question surveys were devised with responses gathered using a 5-point Likert scale; one was tailored to patients (n=50) undergoing the operation and the second was for surgeons (n=30) performing the cases. The patients completed their questionnaire prior to their operation on the day of surgery, whereas the surgeons completed their questionnaires at a later date.
3. Results
Questionnaire response rate was 58% for patients (29/50) and 53.3% for surgeons (16/30), comprising 9 consultants, 5 registrars and 2 unrecorded/other.
14 patients stated they would prefer the surgeon who saw them in the outpatient setting to proceed to perform the operation, with 64.2% (9/14) reporting that they would delay their operation to achieve this. Many of these, 28.6% (4/14), would delay for 2 weeks or more, but only 14.3% (2/14) would be willing to delay for 3 weeks or more (Fig 1). 81% (13/16) of the surgeons felt patients would prefer the surgeon who saw them in the clinic to carry out their operation.
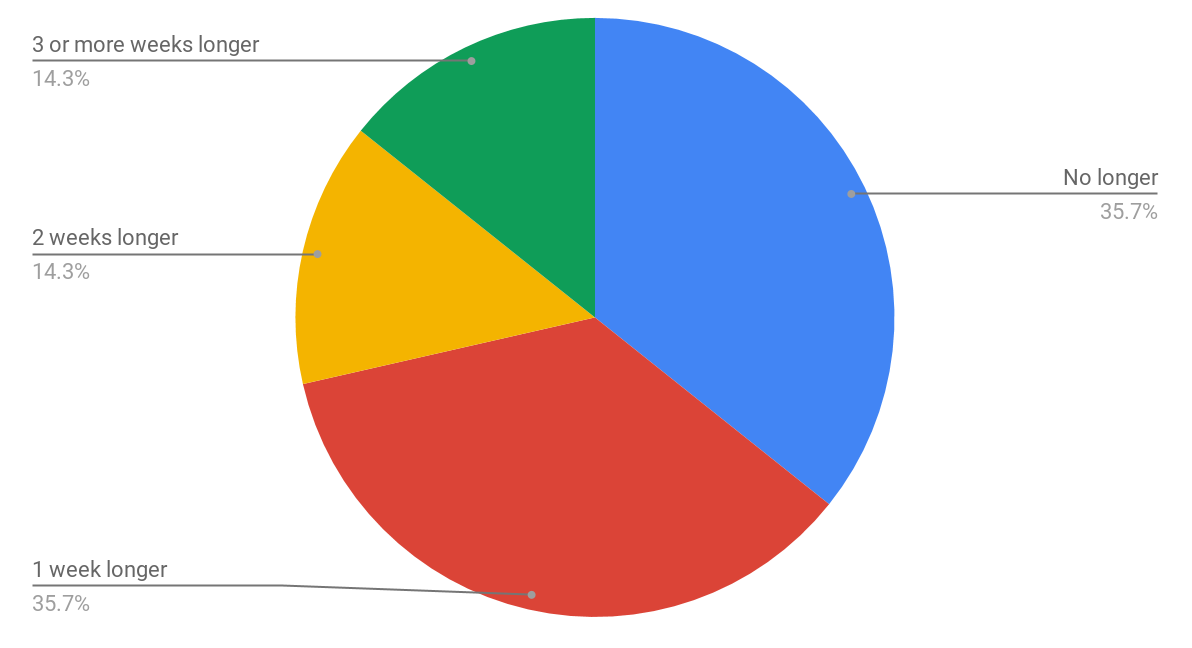
Figure 1: Pie chart representing the length of time that patients would be willing to wait for the same surgeon.
Regarding the consent process, 41.4% (12/29) patients felt that the discussion and subsequent signing of the form spanned both outpatient clinic and the day of surgery, with a further 20.7% (6/29) patients feeling they consented to the operation in the outpatient setting, with the surgeon at that time (Fig 2).
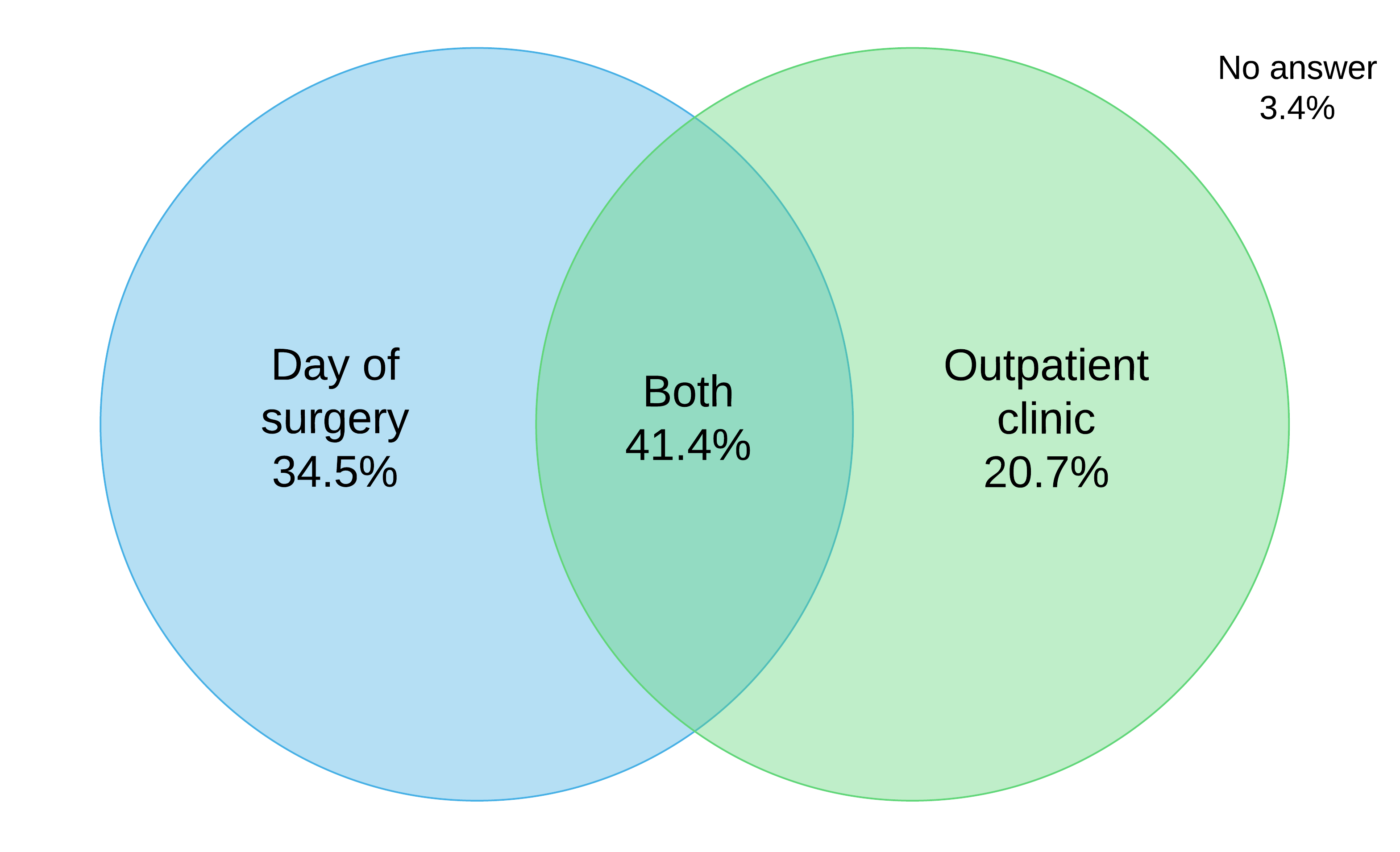
Figure 2: Venn diagram representing at what stage patients felt that they gave consent for the procedure.
4. Discussion
It is widely accepted that patients prefer continuity of care [2][3][4]. The importance of continuity of care is well documented in areas such as general practice [5], caring for vulnerable patients [6] and palliative care for dementia sufferers [7], yet patients often report difficulty in obtaining it [8]. This is likely because using different physicians confers greater flexibility in a service and reduces waiting times, and a general perception that this is more efficient. However, evidence suggests that discontinuity of the healthcare provider in general practice, in fact, led to higher overall health care costs [9]. There is controversy over whether patients prefer fast access to general practice services or would rather wait longer to see the doctor of their choice, with discrete choice experiments giving conflicting results [10][11].
Understanding of continuity of care in elective day case surgery is even less clear, as little work has been carried out in this area. The relative time span of the doctor-patient relationship is much shorter than in general practice or palliative care, often spanning simply an outpatient appointment and the surgery itself (occasionally just the latter). Elective hernia repair patients tend to forget a good deal of what they are told in the outpatient appointment [12] which may impact the consent process. For consent to be valid the patient must be “competent to take the decision, have received sufficient information to make a decision and not be acting under duress.” Informed consent remains valid indefinitely; this allows consent to be obtained in advance, providing that the patient’s condition has not changed and/or no new information has arisen between the consent discussion and the day of surgery [13].
Although some patients feel that consent carries over from the outpatient setting to the day of operation, doubts may arise on the day of surgery and the patient may feel pressured to proceed. It may be beneficial for the patient to see the same surgeon who can recall and address concerns and important issues for an individual patient and confirm consent remains valid. The patient places a high degree of trust upon the surgeon, which makes continuity of greater importance but this requires balance. Changes in operating personnel may decrease waiting times [14] but can heighten patient anxiety, which is already a significant aspect of day case surgery [15].
This study is limited by its small sample size. As well as this, all patients in this sample were undergoing the same operation. As a result, it is not certain that these results are representative of day case operations as a whole, and more research is needed to understand to what extent these results are generalisable.
5. Conclusion
In the context of balancing continuity of care against the speed of service, more patients prioritise being treated quickly, in the context of elective hernia repair. Results obtained in this small study would suggest that a significant group of patients would prefer to be operated on by the same surgeon they originally saw in the outpatient clinic, but would not be willing to delay their operation for a significant length of time. There is a potential gap in perception between surgeons and patients which highlights the need to ask patients about their priorities at the entry point into the secondary care service.
6. Supplementary Materials
Download Patient Questionnaire
Download Surgeon Questionnaire
7. References
[1] Conner-Spady, B. et al. Willingness of patients to change surgeons for a shorter waiting time for joint arthroplasty. CMAJ Can. Med. Assoc. J. J. Assoc. Medicale Can. 2008;179, 327-332.
[2] Mihill, C. Shaping Tomorrow: Issues Facing General Practice in the New Millennium. BMA, 2000.
[3] Fan, V. S., Burman, M., McDonell, M. B. & Fihn, S. D. Continuity of care and other determinants of patient satisfaction with primary care. J. Gen. Intern. Med. 2005;20:226-233.
[4] Haggerty, J. L. et al. Continuity of care: a multidisciplinary review. BMJ. 2003;327: 1219-1221.
[5] Lee, J.-H. et al. Association of the length of doctor-patient relationship with primary care quality in seven family practices in Korea. J. Korean Med. Sci. 2013;28:508-515.
[6] Nutting, P. A., Goodwin, M. A., Flocke, S. A., Zyzanski, S. J. & Stange, K. C. Continuity of primary care: to whom does it matter and when? Ann. Fam. Med. 2003;1:149-155.
[7] Van der Steen, J. T. et al. White paper defining optimal palliative care in older people with dementia: A Delphi study and recommendations from the European Association for Palliative Care. Palliat. Med. 2013. doi:10.1177/0269216313493685
[8] Baker, R. et al. Interpersonal continuity of care: a cross-sectional survey of primary care patients’ preferences and their experiences. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 2007;57:283-289.
[9] De Maeseneer, J. M., De Prins, L., Gosset, C. & Heyerick, J. Provider continuity in family medicine: does it make a difference for total health care costs? Ann. Fam. Med. 2003;1:144-148.
[10] Gerard, K., Salisbury, C., Street, D., Pope, C. & Baxter, H. Is fast access to general practice all that should matter? A discrete choice experiment of patients’ preferences. J. Health Serv. Res. Policy 13 Suppl. 2008;2:3-10.
[11] Rubin, G., Bate, A., George, A., Shackley, P. & Hall, N. Preferences for access to the GP: a discrete choice experiment. Br. J. Gen. Pr. J. R. Coll. Gen. Pr. 2006;56:743-748.
[12] Uzzaman, M. M. et al. Evaluation of patient’s understanding and recall of the consent process after open inguinal hernia repairs. Int. J. Surg. Lond. Engl. 2012;10:5-10.
[13] Anderson, O.A. and Wearne, I.M.J., 2007. Informed consent for elective surgery–what is best practice?~J R S M.~100(2), pp.97-100.
[14] Love, M. M. & Mainous, A. G., 3rd. Commitment to a regular physician: how long will patients wait to see their own physician for acute illness? J. Fam. Pract. 1999;48:202-207.
[15] Mitchell, M. Patient anxiety and modern elective surgery: a literature review. J. Clin. Nurs. 2003;12:806-815.
Article photo credit: COMSEVENTHFLT
- Log in to post comments










