Variation in management of breast lesions with ultrasound appearances typical of a fibroadenoma
1. INTRODUCTION
Conventionally, all women presenting with a palpable breast lesion undergo a triple assessment, consisting of clinical examination, imaging and needle biopsy. Mammography is usually used in older women, while ultrasound is the imaging test of choice in younger women as their denser breast tissue limits mammographic sensitivity [1].
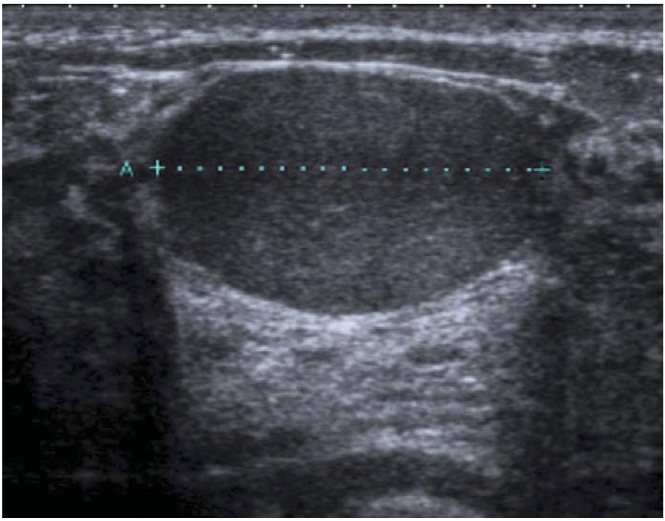
Fibroadenomas are the commonest type of breast lesion, with incidence peaking in women aged 20-24 years [2] They arise in breast lobules and are composed of fibrous and epithelial tissue. They are benign and do not confer an increased risk of breast cancer. On examination fibroadenomas are firm, non-tender, highly mobile lumps. On ultrasound they are typically wider than tall, well defined with smooth edges or fewer than four gentle lobulations, surrounded by a thin echogenic pseudo-capsule and have no other suspicious features (Fig. 1). Diagnostic features on needle biopsy are abundant stromal cells and sheets of uniform-sized epithelial cells that are classically arranged in an antler-like or honeycomb pattern [3].
Figure 1: Ultrasound image of a typical fibroadenoma i.e. a lesion which is wider than tall, well defined with smooth edges or fewer than four gentle lobulations, surrounded by a thin echogenic pseudo-capsule and has no suspicious features.
Previous studies have found that less than 2% of lesions with the typical ultrasound features of a fibroadenoma, are found to be malignant on biopsy [4][5][6][7]. So is biopsy necessary in the large group of women presenting with such lesions? The American College of Radiology Breast Imaging-Reporting and Data System (ACR BI-RADS) guidelines [8], which are commonly used across Europe [9], categorise lesions with a malignancy risk less than 2% as BI-RADS 3 and recommend women undergo short interval follow-up rather than immediate needle biopsy (Table 1). Follow-up reduces cost [1], morbidity [4], and pathology workload [10] compared to biopsy. The full BI-RADS guidelines, which recommend specific management options based on the likelihood of malignancy on imaging, are outlined in Table 1.
Table 1: Breast imaging and reporting data system (BI-RADS) ultrasound categories for breast lesions, with associated malignancy risks and management recommendations [8].
| BI-RADS SCORE | DESCRIPTION | LIKELIHOOD OF MALIGNANCY | MANAGEMENT |
|---|---|---|---|
| 1 | Normal | 0% | Discharge |
| 2 | Benign | Essentially 0% | Discharge |
| 3 | Probably benign | > 0% but ≤ 2% | Short interval follow- up 6 months, 1 year, 2 years |
| 4 | Highly suspicious | > 2% but ≤ 95% | Tissue diagnosis |
| 5 | Malignant | ≥ 95% | 3117.5 |
The UK Royal College of Radiologists Breast Group (RCRBG) has published its own guidelines for managing breast lesions [11]. Women under 25 years who present with lesions with typical ultrasound features of a fibroadenoma are discharged without biopsy or follow-up, whereas those 25 years and above undergo immediate needle biopsy. Equating these recommendations to the BI-RADS system, lesions in women under 25 would be classed as BI-RADS 2 (malignancy risk essentially 0%) and in women over 25 classed as BI-RADS 4 (malignancy risk 2%-95%). There is logic in varying the BI-RADS score and management with patient age; the incidence of breast cancer increases as women get older, so the likelihood that a lesion which looks like a fibroadenoma on ultrasound is actually a cancer in disguise will similarly increase with age. The purpose of this study was to determine current European practice in classifying and managing lesions with ultrasound appearances typical of a fibroadenoma, including how this varied with respect to patient age.
2. MATERIALS AND METHODS
We designed an online questionnaire which was circulated by the European Society of Breast Imaging (EUSOBI) Office to 308 members across 31 European countries. The questionnaire described a lesion that had all the ultrasound appearances typical of a fibroadenoma and also included an ultrasound image of a lesion that met these criteria (Fig. 1). It was specified that the lesion was not suspicious on clinical examination and the woman had no compounding circumstances (known BRCA1 or BRCA2 mutation/family history of breast cancer).
Members were asked how their centre would manage such a lesion in women in each of seven age groups (<15, 15-19, 20-24, 25-29, 30-34, 35-39, 40 and above). Questions included whether mammography would be used, whether needle biopsy would be undertaken, and whether the patient would be discharged or followed up on completion of the evaluation. We asked what BI-RADS score would be given to the lesion, to assess how this score varied with respect to patient age and how it determined management. Details about each centre were also collected, including the country in which it was based, type of centre (academic, state run, privately financed) and the number of patients seen annually.
3. RESULTS
Completed responses were received from members of 33 centres across 18 countries (6 UK and 27 non-UK), comprising a 10.7% response rate. The majority of members (28, 84.8%) were from centres which saw more than 2000 patients annually. 16 (48.5%) centres were academic, 13 (39.4%) state-run and 4 (12.1%) privately financed. Women over 40 years underwent mammography in all centres. The majority of centres (17, 51.5%) did not routinely undertake mammography women aged 35-39. We have therefore presented the data for women up to 39 years to reflect management based almost exclusively on ultrasound findings. Because the 6 UK centres use the RCRBG rather than BI-RADS classification system, these centres are not included in data relating to BI-RADS scoring.
3.1 BI-RADS scoring in relation to age
Of the 27 European centres (not UK), 48% did not change the BI-RADS score of a lesion with the typical ultrasound appearance of a fibroadenoma depending on the patients age, while 41% allocated a higher BI-RADS score to such lesions in older women. The remaining 11% of centres allocated a higher BI-RADS score to the lesion in both older women and very young women (Fig. 2a). Even among centres that used the same pattern of scoring there was variation in the numerical score they gave the lesion, and the specific patient age(s) beyond which the score was increased. As such, there was significant variation in the BI-RADS score given to the same lesion at each patient age (Fig. 2b).
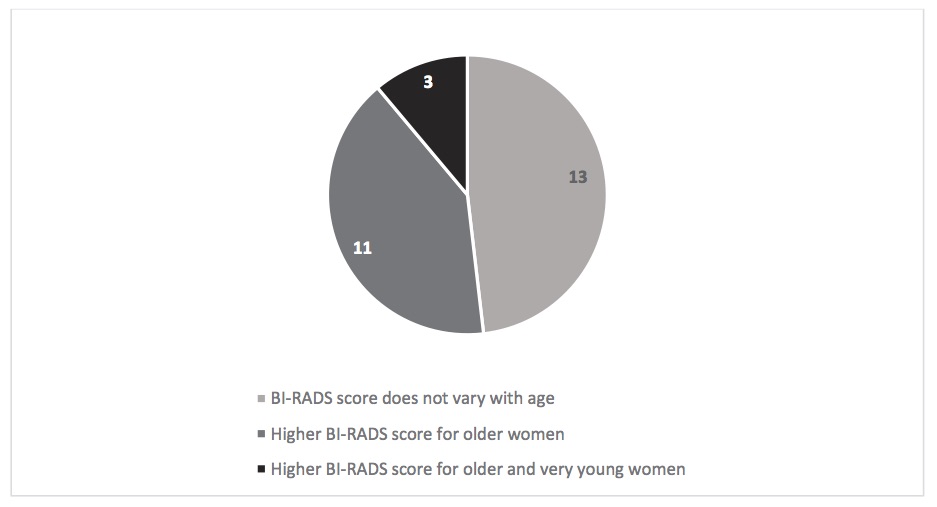
Figure 2a: Pattern in allocating BI-RADS score to an ultrasound image typical of a fibroadenoma with respect to patient age, from 27 European centres.
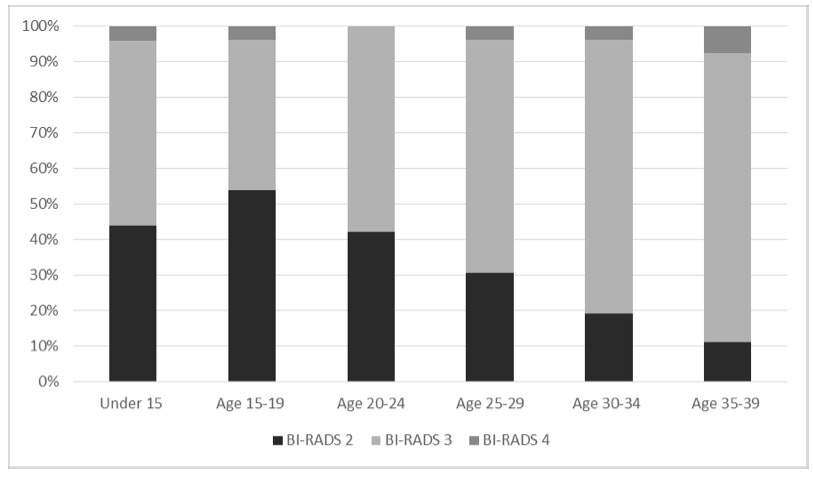
Figure 2b: BI-RADS score allocated to an ultrasound image typical of a fibroadenoma, with respect to patient age.
3.1.1 Management in relation to BI-RADS score:
Amongst the 27 centres, only 33% consistently followed BI-RADS recommendations for management. In 37% of centres management consistently matched recommendations for the BI-RADS score plus one i.e. all lesions scored BI-RADS 2 were followed up and all lesions scored BI-RADS 3 were needle biopsied. In 1 centre (4%) all lesions were scored BI-RADS 2 and needle biopsied. In the remaining 26% of centres there was no consistent relationship between BI-RADS score and management (Fig. 3).
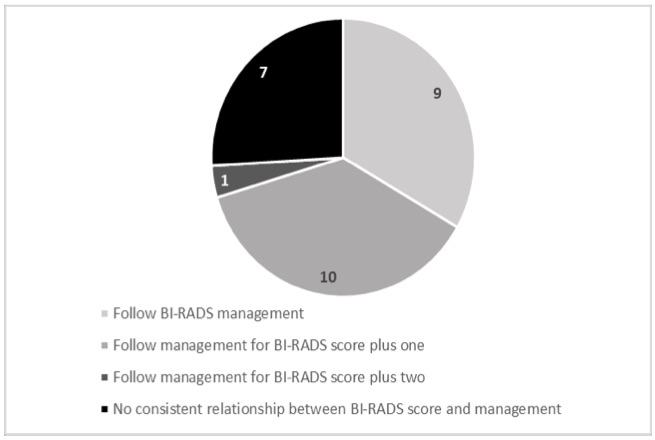
Figure 3: Pattern relating BI-RADS score to management for a lesion with ultrasound appearances typical of a fibroadenoma, from 27 European centres.
3.1.2 Management in relation to age:
Of the 33 centres surveyed (including the 6 UK centres), 18.5% needle biopsied all lesions with the ultrasound appearance typical of a fibroadenoma, irrespective of patient age. 36% did not biopsy any such lesions. 45.5% only needle biopsied older women and the remaining 3% (1 centre) biopsied both very young and older women (Fig. 4a).
Of the 21 centres who biopsied lesions in at least some women, 57% followed up women after a benign biopsy result while 43% discharged women post negative biopsy. Of the 28 centres that did not always biopsy lesions, 64% followed up all women who were not biopsied, 11% only followed up older women, and 25% discharged women who were not biopsied.
Overall there was huge variation in how lesions with ultrasound appearances typical of a fibroadenoma were managed at each patient age (Fig. 4b). Notably, the 6 UK centres (which are included in the above results) uniformly adhered to current UK guidelines. Women under 25 years were discharged without follow-up and women 25 years and over underwent needle biopsy and were discharged following a benign result.
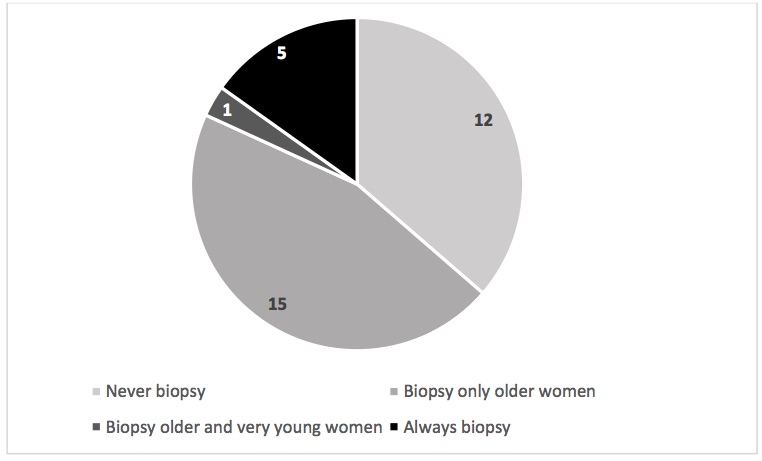
Figure 4a: Patterns of management of lesions with ultrasound appearances typical of a fibroadenoma, from 33 European centres.
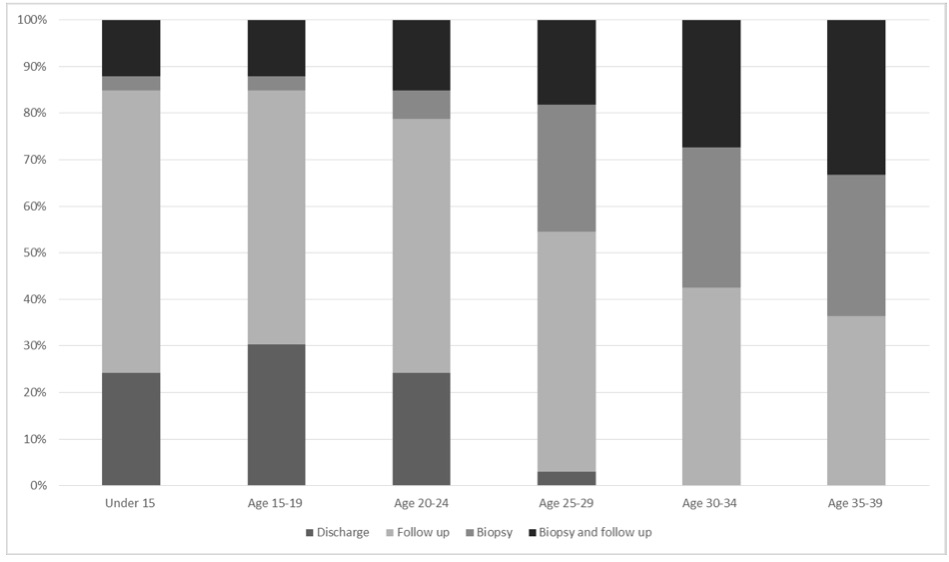
Figure 4b: Management of a lesion with ultrasound appearances typical of a fibroadenoma in 33 European centres, in relation to patient age.
4. DISCUSSION
Our survey is the first review of the management of breast lesions with ultrasound appearances typical of a fibroadenoma across Europe and reveals wide variation in practice. As fibroadenomas are extremely common in young women and the investigation of this benign condition consumes a large amount of healthcare resources, rationalisation of management is much needed.
The survey highlights two potential reasons for this variation in management. The first is a lack of clarity regarding the risk of malignancy of a lesion with ultrasound appearances typical of a fibroadenoma in different age groups. This is evidenced by the fact that centres assign different BI-RADS scores, corresponding to different malignancy risk, to lesions in women of the same age. So, what does current literature suggest is best practice? In women under 25 years the incidence of breast cancer is extremely low and several studies have shown that in this age group a lesion which looks like a typical fibroadenoma on ultrasound is almost never malignant [7][12]. Hence, these lesions would most appropriately be classed as BI-RADS 2 (malignancy risk essentially 0%), with recommended management to directly discharge women. This aligns with the current UK RCRBG guidelines, which recommends women under 25 are discharged without biopsy or follow up [11]. More recent studies have found that the risk of a cancer masquerading as a typical fibroadenomas on ultrasound is similarly close to 0% in women aged 25-30 years [1][13], suggesting that these lesions should also be classified as BI-RADS 2. Accordingly, some centres, including the Cambridge Breast Unit, have moved to discharging women under 30 without biopsy or follow-up [13]. Of course, all women who are discharged must be appropriately safety-netted and breast lesions in women with a significant family history or with suspicious clinical features still warrant further investigation. What about older women? Studies looking at lesions with ultrasound appearances typical of a fibroadenoma across women of all ages have found that the overall risk of malignancy is less than 2% [4][5][6]. So arguably these lesions should be classified as BI-RADS 3, and managed with follow up over 2 years. However there have been no studies specifically looking at women over 30 years. It is possible that the increased incidence of breast cancer with age means the risk of malignancy increases to above 2% in this group. Thus, it may be prudent to classify these lesions as BI-RADS 4 (malignancy risk 2-95%) and biopsy them immediately. Finally, the risk that a histologically benign lesion is actually a cancer is extremely close to 0% [14], indicating that it is unnecessary to follow up women after a negative biopsy result.
A second explanation for the variation in management is that there is disagreement regarding the risk of malignancy above which follow-up or needle biopsy is necessary. Evidence for this includes the fact that 37.0% European centres consistently disregard RADS recommendations and instead follow the recommendations for the BI-RADS score plus one i.e. follow-up of all BI-RADS 2 and needle biopsy of all BI-RADS 3 lesions. Moreover, 36.4% of centres continue to follow-up women even after a benign biopsy result. There are several possible reasons for this cautious approach. Firstly, it is impossible to say with 100% certainty that a lesion is benign. In particular, phyllodes tumours sometimes have similar appearances to fibroadenomas on ultrasound (and rarely even on biopsy) and can occasionally become malignant. Although they are extremely uncommon compared to fibroadenomas, some centres may be unwilling to accept this risk. This is more likely to be the case in countries/centres which are privately funded, meaning there are fewer financial pressures acting to minimise over-investigation. Additionally, patient preference will play a role; Harvey et al. found 22.7% of patients with a palpable lesion preferred needle biopsy to follow-up [4]. Variation in management will also be influenced by variation in who looks after these women. In the UK the diagnostic process usually takes place in a breast clinic with specialised radiographers and radiologists involved in the diagnostic process. In contrast, in some other European countries gynaecologists carry out all steps in the triple assessment. Ultrasound is operator dependent, so practitioners with less specialist experience may be less confident in discharging women without a biopsy.
The main limitation of this study is that the European survey results are based only on 33 centres; these may not be representative of all centres managing fibroadenomas across Europe. However, these were all large, experienced centres, so the inconsistency between them is worth our consideration.
In conclusion, the management of breast lesions with ultrasound appearances typical of a fibroadenoma varies widely across Europe. This appears to be due to both a lack of clarity about how the risk of malignancy varies with patient age, and disagreement about the risk above which needle biopsy or follow-up is necessary. Current literature suggests that the risk of malignancy in women under 30 is so low that the lesion can be classified as BI-RADS 2 and women can be safely discharged without biopsy or follow-up. This would minimise unnecessary cost, morbidity and workload associated with this common, benign condition. Additional multi-centre research quantifying the risk of malignancy in women over 30 is required to determine the appropriate BI-RADS score and thus management. However, this would not address the fact that the majority of European centres do not manage lesions according to the BI-RADS recommendations. This is likely due to a range of economic, social and political factors and means rationalising management across Europe will not be straightforward.
5. ACKNOWLEDGEMENTS
We would like to thank Kathryn Taylor, DCR MSc, Peter Britton MBBS FRCR and Matthew Wallis MBChB FRCR from the Department of Radiology, Cambridge Breast Unit for all their support. We are grateful to EUSOBI for their help with the questionnaire
6. References
[1] Loving V a., DeMartini WB, Eby PR, Gutierrez RL, Peacock S, Lehman CD. Targeted ultrasound in women younger than 30 years with focal breast signs or symptoms: Outcomes analyses and management implications. Am J Roentgenol. 2010;195(6):1472-7.
[2] Guray M, Sahin AA; Benign breast diseases: classification, diagnosis, and management. Oncologist. 2006 May11(5):435-49.
[3] DeMay, M. Practical Principles of Cytopathology (Revised ed.). ASCP Press. p. 2007. ISBN 0-89189-549-3.
[4] Harvey JA, Nicholson BT, LoRusso AP, Cohen MA, Bovbjerg VE. Short-term follow-up of palpable breast lesions with benign imaging features: Evaluation of 375 lesions in 320 women. Am J Roentgenol. 2009;193(6):1723-30.
[5] Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995;196(1):123-34.
[6] Skaane P, Engedal K. Analysis of Sonographic features in the Differentiation of Fibroadenoma and Invasive Ductal Carcinoma. AJR. 1998;170(1):109-14.
[7] Graf O, Helbich TH, Hopf G, Graf C, Sickles EA. Probably benign breast masses at US: Is Follow-up an Acceptable Alternative to Biopsy? 2007;244(1).
[8] Breast imaging reporting and data system (BI-RADS) Atlas- Ultrasound 5th edn. Am Coll Radiol. 2013;121-32.
[9] Taylor K, Britton P, O’Keeffe S, Wallis MG. Quantification of the UK 5-point breast imaging classification and mapping to BI-RADS to facilitate comparison with international literature. Br J Radiol. 2011;84(1007):1005-10.
[10] Maxwell AJ, Pearson JM. Criteria for the safe avoidance of needle sampling in young women with solid breast masses. Clin Radiol. 2010;65(3):218-22.
[11] Willett AM, Michell MJ, Lee MJR. Best practice diagnostic guidelines for patients presenting with breast symptoms. 2012;(November):1-60.
[12] Smith G, Burrows P. Ultrasound diagnosis of fibroadenoma, is biopsy always necessary? Clin Radiol. 2008;63:511-5.
[13] Taylor K, Britton P, Sonoda L, Sinnatamby R (2009) Is it safe practice not to biopsy fibroadenomas in women under 30?
[14] Wallis M, Tarvidon A, Helbich T, Schreer I. Guidelines from the European Society of Breast Imaging for diagnostic interventional breast procedures. Eur Radiol. 2007;17(2):581-8.
- Log in to post comments










