Extensive cervical necrotising fasciitis with mediastinitis in a COVID-19 positive patient: a case report

Abstract
Necrotising fasciitis is a rapidly progressing soft tissue infection associated with significant morbidity and mortality. We present a case of cervical necrotising fasciitis with mediastinal extension in a diabetic young male who was COVID-19 positive. He presented with a five-day history of left-sided neck swelling which was fluctuant, red and painful. Subsequent debridement and management of the wound were complicated by the comorbid SARS-CoV2 infection due to potential need for proning. This case highlights the complex interplay between the management of two significant conditions; the surgical approach to necrotising fasciitis and the concern of deterioration due to COVID-19.
Key Messages
• Necrotising fasciitis is a rare and life-threatening soft tissue infection most commonly seen in the abdomen and perineal regions; it very rarely occurs in the cervicofacial region
• Bacterial culprits for necrotising fasciitis tend to be polymicrobial however cases involving only Beta-haemolytic streptococci are possible
• The use of early and aggressive surgical debridement is essential in containing necrotising soft tissue infections and serves as the most important tool in combating the high morbidity and mortality rates
• A cellulitis that is not responsive to antibiotic therapy should increase suspicion that necrotising fasciitis could be the underlying issue
• There is the possibility that underlying COVID-19 infection can predispose to necrotising fasciitis, and has impacts on management due to potential need for proning in severe COVID-19 infection
Introduction
Necrotising soft tissue infections are a spectrum of rapidly progressing soft tissue necrosis associated with significant morbidity and mortality. Whilst necrotising fasciitis is well characterised in the abdominal wall, perineum and lower extremities; the chest wall serves as a very rare location for necrotising fasciitis to take hold.[1] Necrotising fasciitis is most commonly polymicrobial with Bacteroides, streptococci and gram-negative Enterobacteriaceae often isolated.[2] There can however be a single pathogen involved, for which Beta-haemolytic streptococci are often the culprit; hence its coined name of ‘flesh-eating bacterium’.[3]
The rapid identification of necrotising fasciitis is essential in reducing associated mortality. Findings such as pain out of proportion to skin changes, oedema extending beyond erythematous skin and a wooden-hard texture can differentiate necrotising fasciitis from cellulitis.[4] The finger test is a useful preliminary investigation, in which the dissection of tissue with minimal resistance is considered a positive result.[5] The LRINEC (Laboratory Risk Indicator for NECrotising fasciitis score) is useful both for the diagnosis of necrotising fasciitis and prognosis.[6]
In this case, the presence of both cervical and chest necrotising fasciitis on a background of COVID-19 infection represents a particularly challenging case in terms of management. Given the widespread nature of the current COVID-19 pandemic, understanding potential bacterial superinfection as a complication and how to manage it has never been more essential in the medical discourse.
Case History
A 40-year-old diabetic male was admitted to the emergency department (ED) with a five-day history of left-sided neck swelling at the angle of the mandible extending down the left side of the neck onto his chest. He had been self-isolating at home due to a sore throat with suspected COVID-19 and was taking metformin and ramipril for his Type 2 diabetes mellitus (T2DM) and hypertension (HTN), respectively. He had presented to his general practitioner with dysphagia and throat swelling that did not respond to prescribed co-amoxiclav. The symptoms progressively worsened and at presentation, to the ED the mass was fluctuant, red and painful. There was no trismus or intraoral evidence of infection. He was pyrexial (T38.3), hypotensive and tachycardic (123) with signs of systemic infection (lactate 4.1). He was subsequently transferred to ICU due to haemodynamic instability and suspected necrotising fasciitis.
On admission, routine bloods revealed a raised total white cell count (15.5X10*9/L) and a lymphopenia (0.71x 10*9/L), with poor glycaemic control. His Arterial Blood gas is shown in Figure 1. A computed tomography (CT) neck and chest were performed which revealed extensive inflammatory changes comprising cellulitis fluid (Figure 2). The patient was taken to theatre for exploration and debridement and on examination, there was extensive gas, tissue necrosis and tissue liquefaction from level II-V of the neck up to the anterior chest wall. An examination under anaesthetic was performed, and there was estimated to be 5% body surface area (BSA) soft tissue loss in the upper chest and left neck (Figure 3). There was extensive myonecrosis of both residual pectoralis major muscles with skip lesions throughout. Blood cultures performed on initial presentation to ICU displayed Group B strep (Streptococcus agalactiae).
COVID positive status was confirmed. This prevented the use of free flap reconstruction in case the patient deteriorated from a COVID standpoint and proning was required in the near future. There were concerns regarding proning interfering with the free-flap aftercare and the increased risk of flap associated complications. Therefore, grafting of the area was performed on day 7 of admission. By that evening, his lymphopenia worsened (0.6 x10*9/L) and his respiratory symptoms progressed with a significantly elevated D-dimer (478).
On day 8 of admission, the patient was intubated due to acute shortness of breath with tachycardia, and coughing with +++secretions. There were crepitations in the right lung base and reduced air entry bilaterally. A chest x-ray (CXR) performed demonstrated bilateral ground-glass opacities but no significant collapse. On day 10 in ICU, the patient was extubated successfully and remained stable. He remained in hospital recovering from the infection but was stable enough to be stepped down from ICU. On the ward, he made good progress with physiotherapy to clear extensive secretions in the upper airways. He subsequently developed mucous plugging and a small pleural effusion and was stable on 3L O2. He was speaking in full sentences and not in any respiratory distress. The patient significantly improved over the following weeks, with his grafts healing appropriately (Figure 4). He went on to develop a scar contracture on his left neck from the skin grafting, but with regular physiotherapy is making improvements in overall quality of life.
Discussion
Whilst cervicofacial cases of necrotising fasciitis are rare, they are usually explained by the oral cavity being the nidus of infection. What is unusual in this case is the lack of a clear focus of the infection, with the sore throat attributed to his infection with SARS-CoV2. The presence of poorly controlled diabetes as a comorbidity in this patient is significant, as evidence suggests that diabetes can predispose to necrotising fasciitis.[7] The typical symptomatic triad of necrotising fasciitis is erythema, fever and pain all of which were present in our patient.[8] The presence of soft tissue gas is a classic sign, and was present both radiologically (Figure 2) and clinically in theatre on debridement.
Overall case-fatality rates of necrotising fasciitis vary but are estimated to be around 16.4% in community-acquired necrotising soft tissue infections.[9] This mortality rate increases in infections affecting the head and neck, especially in cases of thoracic extension as occurred in our patient.[10] Reducing this mortality rate is dependent on early recognition of the disease. The relationship between the patients COVID-19 infection and the development of necrotising fasciitis are unclear, however, there have been reports of dermatological manifestations of COVID-19.[11] The presence of necrosis or livedo was found in 6% of patients in a Spanish nationwide study, and could potentially bridge the gap between the preceding SARS-CoV2 infection and the onset of necrotising fasciitis. The COVID-19 related dermatological manifestations affect the barrier to pathogens that the skin offers, thus predisposing to infections such as necrotising fasciitis. Additionally the lymphopenia in this patient, in combination with the poor glycaemic control, may have both contributed to the patients' susceptibility to infection.
A key challenge with this case was balancing the management of necrotising fasciitis with the concomitant COVID-19 infection, as the risk of progression requiring proning meant that a free flap could not be performed.
Whilst not confirmed, this case could represent a bacterial superinfection secondary to COVID-19 infection, as it would appear the symptoms of SARS-CoV2 preceded the dermatological manifestation of his necrotising fasciitis. The lymphopenia associated with COVID-19 can predispose to infection, and a combination of diabetes and lymphopenia should warrant concern for bacterial superinfection.
Informed written patient consent has been obtained for the use of information and images for the purposes of this case report.
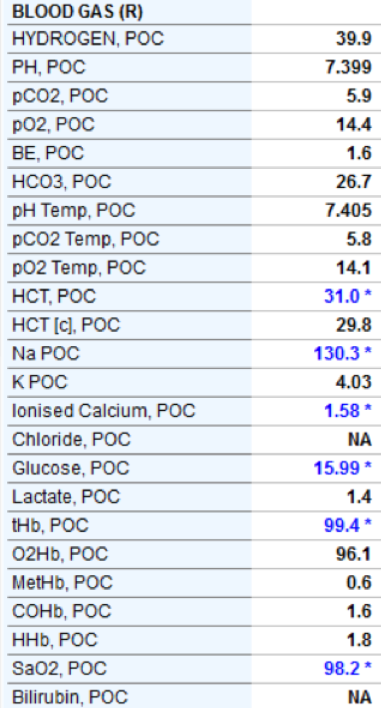
Figure 1: Arterial Blood Gas
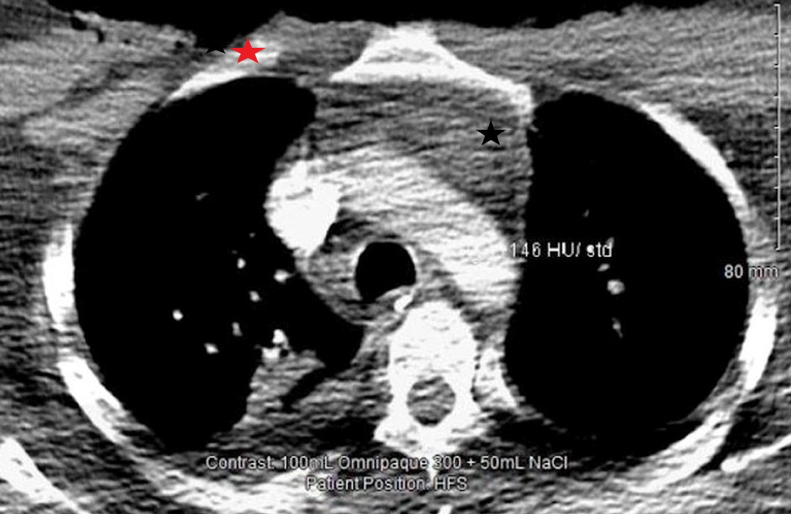
Figure 2: Day 2 ICU
CT neck and thorax with contrast.
There is persisting subcutaneous induration and oedema in the visceral compartment of the neck on the left side (red star), with swelling and induration of the anterior mediastinal fat (black star).

Figure 3: Extensive debridement performed for necrotising fasciitis of neck, anterior upper chest wall & mediastinitis

Figure 4: 28 days after debridement there is adequate healing of skin graft with some dry areas.
References
[1] Urschel JD, Takita H, Antkowiak JG. Necrotizing soft tissue infections of the chest wall. The Annals of thoracic surgery. 1997 Jul 1;64(1):276-9.
[2] Elliott D, Kufera JA, Myers RA. The microbiology of necrotizing soft tissue infections. The American journal of surgery. 2000 May 15;179(5):361-6.
[3] Stevens DL. The flesh-eating bacterium: what's next?. The Journal of infectious diseases. 1999 Mar 1;179(Supplement_2):S366-74.
[4] Andreasen, T.J., Green, S.D. and Childers, B.J., 2001. Massive infectious soft-tissue injury: diagnosis and management of necrotizing fasciitis and purpura fulminans. Plastic and Reconstructive Surgery, 107(4), pp.1025-1036.
[5] Puvanendran, R., Huey, J.C.M. and Pasupathy, S., 2009. Necrotizing fasciitis. Canadian Family Physician, 55(10), pp.981-987.
[6] Su, Y.C., Chen, H.W., Hong, Y.C., Chen, C.T., Hsiao, C.T. and Chen, I.C., 2008. Laboratory risk indicator for necrotizing fasciitis score and the outcomes. ANZ journal of surgery, 78(11), pp.968-972.
[7] Fazeli MS, Keramati MR. Necrotizing fascitis: an epidemiologic study of 102 cases. Indian Journal of Surgery. 2007 Aug 1;69(4):136-9.
[8] Wang JM, Lim HK. Necrotizing fasciitis: eight-year experience and literature review. The Brazilian Journal of Infectious Diseases. 2014 Mar 1;18(2):137-43.
[9] Frazee BW, Fee C, Lynn J, Wang R, Bostrom A, Hargis C, Moore P. Community-acquired necrotizing soft tissue infections: a review of 122 cases presenting to a single emergency department over 12 years. The Journal of emergency medicine. 2008 Feb 1;34(2):139-46.
[10] Mao JC, Carron MA, Fountain KR, Stachler RJ, Yoo GH, Mathog RH, Coticchia JM. Craniocervical necrotizing fasciitis with and without thoracic extension: management strategies and outcome. American journal of otolaryngology. 2009 Jan 1;30(1):17-23.
[11] Galván Casas C, Catala AC, Carretero Hernández G, Rodríguez‐Jiménez P, Fernández‐Nieto D, Rodríguez‐Villa Lario A, Navarro Fernández I, Ruiz‐Villaverde R, Falkenhain‐López D, Llamas Velasco M, García‐Gavín J. Classification of the cutaneous manifestations of COVID‐19: a rapid prospective nationwide consensus study in Spain with 375 cases. British Journal of Dermatology. 2020 Jul;183(1):71-7.
Article Photo Credit: Image by Sasin Tipchai from Pixabay
- Log in to post comments










